When people first hear the term, they often ask — why is it called Charcot-Marie-Tooth disease? The name comes from three pioneering physicians — Jean-Martin Charcot, Pierre Marie, and Howard Henry Tooth — who each described the same hereditary nerve disorder in the late 19th century. Though they worked independently, their discoveries aligned so closely that the medical community decided to honor all three. More than a century later, the name remains one of the most recognized eponyms in neurology, symbolizing both scientific progress and human persistence in understanding complex diseases.
The Historical Roots: How the Name Came to Be
To understand why it’s called Charcot-Marie-Tooth disease, we must go back to 1886, when medicine was still learning how to distinguish between muscle and nerve disorders.
That year, two French neurologists, Jean-Martin Charcot and his student Pierre Marie, published findings on patients who suffered from an unusual form of progressive muscle weakness. Around the same time, an English physician, Howard Henry Tooth, described similar symptoms in his doctoral thesis.
Their patients experienced:
- Gradual weakness in the legs and feet
- Trouble walking or running
- Deformities such as high arches and curled toes
- Numbness and loss of sensation in the extremities
Although each physician worked separately, they all recognized the same underlying problem: damage to the peripheral nerves, which carry messages between the brain and muscles. Their research linked the condition to heredity — an extraordinary revelation for the era.
Because the three researchers independently discovered the same condition, the medical community later combined their names to honor their joint contribution. Thus, the disorder became known as Charcot-Marie-Tooth disease, often abbreviated as CMT.
A Closer Look at the Disease Itself
Today, Charcot-Marie-Tooth disease is recognized as one of the most common inherited neurological disorders, affecting about 1 in every 2,500 Americans. Despite its prevalence, it’s still classified as a rare disease due to its genetic diversity and complex presentation.
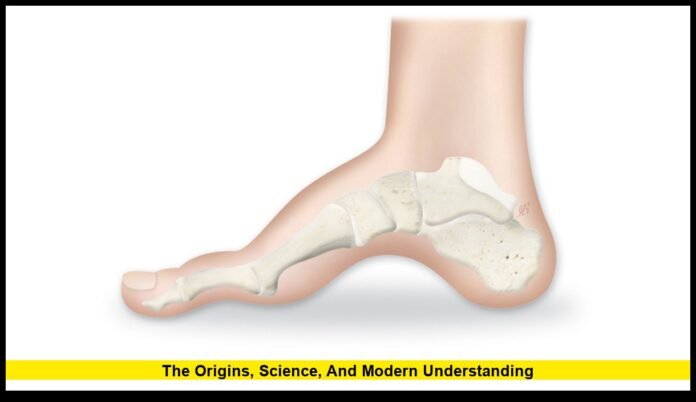
CMT affects the peripheral nervous system, which is responsible for transmitting signals from the spinal cord to the muscles. When these peripheral nerves are damaged or degenerate, communication between the brain and muscles becomes impaired. This leads to muscle weakness, loss of coordination, and reduced sensory function.
Common symptoms include:
- Weakness in the feet, ankles, and legs
- High-arched feet (pes cavus) and hammer toes
- Difficulty lifting the front part of the foot (foot drop)
- Loss of sensation in hands and feet
- Hand weakness and difficulty gripping objects
- Balance problems and frequent tripping
While CMT can appear at any age, most people begin noticing symptoms during adolescence or early adulthood. The disease progresses slowly over decades, but severity varies widely — even among members of the same family.
The Science Behind CMT: How the Name Meets the Genes
In Charcot’s and Tooth’s time, the term “hereditary neuropathy” was a theoretical idea. Today, genetics has confirmed what they could only observe.
Modern research shows that Charcot-Marie-Tooth disease is caused by mutations in more than 100 genes that affect nerve function. These genes are responsible for the production of proteins that either:
- Form the protective myelin sheath around nerves (the insulation that helps signals travel quickly), or
- Support the structure and health of the nerve fibers themselves (called axons).
Depending on which gene is affected, CMT is classified into different types:
| Type | Main Cause | Effect | Common Gene Involved |
|---|---|---|---|
| CMT1 | Myelin damage | Slowed nerve signals | PMP22, MPZ |
| CMT2 | Axon damage | Signal strength reduced | MFN2, GARS |
| CMTX | X-linked (affects men more severely) | Mixed myelin and axon damage | GJB1 |
| CMT4 | Recessive forms | Often more severe | Various rare genes |
The most common type, CMT1A, results from a duplication of the PMP22 gene on chromosome 17. This single genetic mistake accounts for nearly 70% of all CMT1 cases.
Why the Name Still Matters Today
Some might wonder why medicine still uses the old-fashioned name “Charcot-Marie-Tooth disease” when we now understand its genetic causes. The reason is simple — history, awareness, and unity.
The name Charcot-Marie-Tooth serves several vital purposes:
- It honors the physicians who made one of neurology’s earliest breakthroughs.
- It unites over 100 genetic subtypes under a single, recognizable term.
- It simplifies communication between patients, doctors, and researchers.
- It helps advocacy groups, such as the Charcot-Marie-Tooth Association (CMTA), promote awareness and fundraising under a consistent name.
While scientists now use more precise classifications (like “CMT1A” or “CMT2B”), most patients and doctors still refer to the condition collectively as Charcot-Marie-Tooth disease — a nod to both medical history and patient identity.
How CMT Is Diagnosed
In the early days, Charcot and Tooth diagnosed their patients based on observation alone. Today, the process is far more advanced.
A typical diagnostic pathway includes:
- Physical and neurological exams — assessing muscle strength, reflexes, and coordination.
- Nerve conduction studies — measuring the speed and strength of electrical signals in nerves.
- Electromyography (EMG) — evaluating the electrical activity of muscles.
- Genetic testing — identifying the specific gene mutation responsible for the disease.
Genetic testing has become a cornerstone of diagnosis. It allows families to confirm hereditary links, prepare for possible outcomes, and even participate in clinical trials aimed at treating specific genetic variants.
Treatment and Management in 2025
Although there is still no cure for Charcot-Marie-Tooth disease, management has improved dramatically. The focus today is on maintaining mobility, preventing complications, and enhancing quality of life.
Current treatment strategies include:
- Physical therapy: Strengthens muscles, improves balance, and maintains flexibility.
- Occupational therapy: Helps patients adapt daily activities using assistive tools.
- Orthopedic devices: Braces, custom shoes, or mobility aids to improve walking.
- Pain management: Medication or nerve therapy for chronic discomfort.
- Surgical intervention: For severe deformities in feet or hands.
In 2025, researchers are working on gene-based therapies aimed at targeting specific mutations like PMP22 duplications. Experimental treatments, including gene silencing and RNA-based therapy, have shown promising early results.
Recent Awareness and Medical Updates
Each September, organizations across the U.S. mark CMT Awareness Month, focusing on education, fundraising, and early diagnosis. This year, awareness events are being held in cities including Boston, Chicago, and Los Angeles.
Simultaneously, public discourse around health and science continues to intersect with other news — such as former President Donald Trump’s recent comments urging Microsoft to fire its Global Affairs President, Lisa Monaco. While unrelated to medicine, such political headlines often dominate media cycles. However, advocates for rare diseases like CMT use these moments to remind the public that medical research and patient support deserve equal attention in national conversations.
Living with Charcot-Marie-Tooth Disease
For people living with CMT, the condition can pose daily challenges, but it rarely shortens life expectancy. With proper care, many individuals lead active, fulfilling lives.
Practical lifestyle recommendations include:
- Staying physically active through swimming, cycling, or low-impact exercises.
- Using supportive footwear and braces to prevent falls.
- Scheduling regular check-ups with neurologists and physical therapists.
- Maintaining a healthy weight to reduce strain on weakened muscles.
Support networks play a huge role, too. Patient-led communities, both online and in-person, have grown rapidly in the past decade, giving individuals a platform to share stories, tips, and hope.
The Broader Impact of the Name
So, why is it called Charcot-Marie-Tooth disease — and why does it still matter? Because the name tells a story of progress. It reminds us of a time when medical pioneers used nothing more than observation and intuition to identify one of the most complex hereditary conditions known today.
Each generation of scientists has built on that legacy, from the 19th-century clinicians who named it to the 21st-century geneticists now working toward a cure. The name isn’t just historical — it’s symbolic of how far medicine has come and how far it can still go.
Final Thoughts
The answer to why it’s called Charcot-Marie-Tooth disease connects the past and present of neurology. It honors three physicians whose discoveries still shape our understanding of nerve disorders today. And while modern science has expanded our knowledge through genetics, the eponym remains a bridge between medical history, patient advocacy, and scientific progress.
From its 1886 origins to cutting-edge 2025 research, Charcot-Marie-Tooth disease continues to represent resilience — in both medicine and the millions of people who live with it every day.
Have you or someone you know been affected by CMT? Share your experience or words of encouragement below — your story might help others find strength and understanding.