A Deep, Fact-Based Look at the Case of the Man Declared Brain-Dead Who Showed Signs of Life in the Operating Room
The phrase wake up dead man has become one of the most discussed medical stories in the United States throughout 2025. It refers to a shocking Kentucky case in which a man who had been declared brain-dead unexpectedly displayed signs of life just moments before organ-retrieval surgery. This disturbing sequence of events has triggered renewed scrutiny of brain-death protocols, ethical concerns surrounding organ donation, and questions about how such a rare incident could occur inside a modern U.S. hospital.
This expanded, fact-based news article details every verified aspect of the incident, how it unfolded, and why it continues to raise national concern in 2025.
The Case Behind the “Wake Up Dead Man” Headline
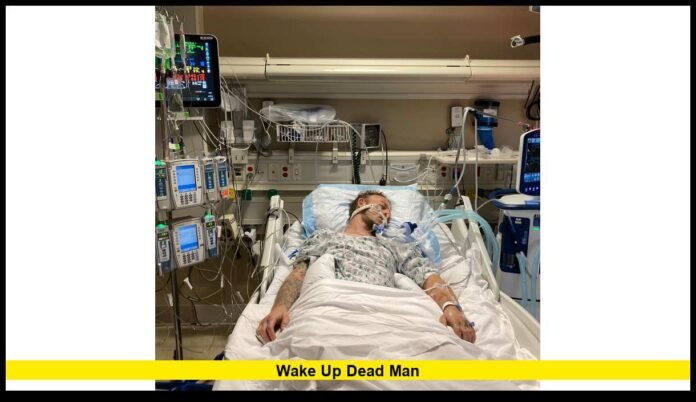
The incident involves Anthony Thomas “TJ” Hoover II, a Kentucky man who suffered a serious medical emergency and was hospitalized with life-threatening complications. He was later declared brain-dead, and plans were made for organ donation in accordance with his donor registration.
However, during the honor walk—a ceremonial procession held for organ donors—family members and medical staff witnessed signs that Hoover might not be deceased. Once inside the operating room, he reportedly opened his eyes, moved, and appeared to shed tears. These reactions stunned the surgical team, and the organ-retrieval procedure was immediately stopped.
Hoover survived the attempted organ procurement and continues to live with significant impairments under family care. The fact that he displayed signs of life during the organ-harvesting preparation is the central reason the case is now widely known as the wake up dead man incident.
Why the Story Returned to the Spotlight in 2025
Although the event originally occurred several years ago, multiple developments in 2025 have brought the story back into national focus:
- Fresh interviews from Hoover’s family, who continue to speak out about what they believe went wrong.
- Increased public attention on medical ethics, especially in the fields of organ donation and end-of-life care.
- New state-level discussions about clarifying brain-death laws, which vary widely across the U.S.
- Growing public concern about trust in hospital decision-making, influenced by viral social media interest in the topic.
As these conversations intensify, the story remains relevant for healthcare professionals, lawmakers, and organ-donor families across the country.
How Brain Death Is Determined—and Where the Case Raised Questions
Understanding the larger discussion requires examining how brain death is normally diagnosed in U.S. hospitals.
Typical Brain-Death Evaluation Includes:
- Confirming irreversible brain injury
- Demonstrating the complete absence of brainstem reflexes
- Conducting apnea testing (determining the body’s inability to breathe independently)
- Ensuring no sedating medications or metabolic factors interfere with evaluations
- Documenting findings thoroughly
- Having a qualified physician complete the certification
The wake up dead man case has caused many to ask whether these steps were properly completed. Families nationwide have expressed concern that variations in hospital procedures could lead to misdiagnoses, even if extremely rare.
The Family’s Experience and Concerns
Throughout 2024 and 2025, Hoover’s family has spoken publicly about their distress, focusing on several concerns surrounding the experience:
- They reported noticing movements and reactions long before the procedure began.
- They questioned whether all required neurological tests were completed.
- They said communication between the hospital and family felt rushed.
- They believed staff dismissed signs that Hoover was still alive.
- They have advocated for stronger protections for patients declared brain-dead.
Their outspokenness has amplified the public’s understanding of the emotional toll that end-of-life decisions can take on families, especially when medical professionals and loved ones disagree.
Why the Incident Has Sparked Nationwide Debate
The implications of a wake up dead man scenario reach far beyond one hospital or one state. It raises questions that resonate nationally.
1. Can Brain-Death Standards Be Strengthened?
Many medical groups believe national guidelines must be unified, as each state has different definitions and procedures. A national standard may reduce inconsistencies.
2. Should There Be Mandatory Independent Evaluators?
Some advocates propose adding a second, unaffiliated physician to verify brain death before organ procurement begins.
3. Do Families Need More Transparent Communication?
Families often rely entirely on hospital staff. A standardized “family briefing protocol” may help reduce confusion or mistrust.
4. Does the Organ Procurement Process Need More Oversight?
Organ donation saves thousands of lives annually, but this case highlights a need for extra verification steps prior to surgery.
Understanding the Organ-Donation Process
To fully grasp how the wake up dead man event occurred, it’s important to understand the typical organ-donation timeline once a patient is declared brain-dead.
Standard Steps Include:
- Official confirmation of brain death
- Notification of the organ-procurement organization
- Family briefing about the donation process
- Scheduling of an honor walk (optional, but common)
- Transfer to surgical staff
- Final verification of legal death
- Organ-retrieval procedure
In Hoover’s case, the crucial moment came when signs of life were observed after the family had agreed to organ retrieval and before the surgery began—precisely the point at which multiple checks should have confirmed death with certainty.
Why Such Incidents Are Extremely Rare
Medical experts emphasize that cases like this are extraordinarily uncommon. Brain death is considered as definitive as cardiac death, and organ donation almost always proceeds only after multiple independent evaluations.
Yet the rarity of such an event does not diminish its seriousness. Even one failure can undermine public trust, which is why hospitals, organ-procurement agencies, and lawmakers are now discussing potential reforms.
Public Reactions and Ethical Concerns
Throughout 2025, social media platforms and national discussions have highlighted significant ethical concerns related to the case.
Top Issues Shaping Public Opinion:
- Is the pressure to secure organs influencing the pace of death declarations?
- Are families being allowed enough time to process medical information?
- Should oversight of organ procurement be increased?
- Are hospitals relying too heavily on outdated or inconsistent brain-death standards?
While hospitals and organ-donation networks strongly deny any improper pressure, the debate continues to unfold.
Discussions in the Medical Community
Healthcare professionals have taken varied positions in response to the wake up dead man event.
Many doctors argue:
- Brain death remains a clear, evidence-based diagnosis.
- The overwhelming majority of organ donations follow strict rules.
- Emotionally charged cases can distort the public’s understanding of medical facts.
Others say:
- The system needs modernization and consistency.
- More oversight could protect both patients and organ donation credibility.
- Families deserve broader rights to request additional testing.
The medical community acknowledges that while the system works well for most patients, improvements could prevent rare failures.
How Families Can Protect Themselves in Serious Medical Situations
Americans considering organ donation or facing difficult end-of-life decisions can take steps to safeguard themselves.
Recommended Actions:
- Ask for a detailed explanation of brain-death criteria used by the hospital.
- Request multiple neurological examinations.
- Ask whether sedative medications could still be affecting the patient.
- Request a second medical opinion if anything seems unclear.
- Document every conversation with care teams.
These steps support informed decision-making at an emotionally overwhelming time.
Possible Reforms Being Discussed in 2025
Because of the renewed focus from the wake up dead man case, several potential reforms are being evaluated across the U.S.
Ideas Under Consideration:
- A standardized federal definition of brain death
- Mandatory multi-doctor verification before organ retrieval
- Real-time monitoring during honor walks and pre-surgical checks
- Additional training for hospital staff
- New protocols ensuring families are never rushed
These discussions remain ongoing.
Final Thoughts
The wake up dead man case is one of the most unsettling medical stories in recent years, not because it reflects the norm but because it exposes gaps in a system that must function flawlessly. While organ donation is vital and overwhelmingly safe, this case reminds the country that human oversight must never be taken lightly. As 2025 continues, the debate surrounding patient rights, medical accuracy, and ethical practices is likely to shape new policies aimed at restoring trust and preventing similar incidents.
If you have thoughts, concerns, or questions about organ donation or brain-death protocols, share your perspective below—your voice is part of a conversation that matters to families nationwide.