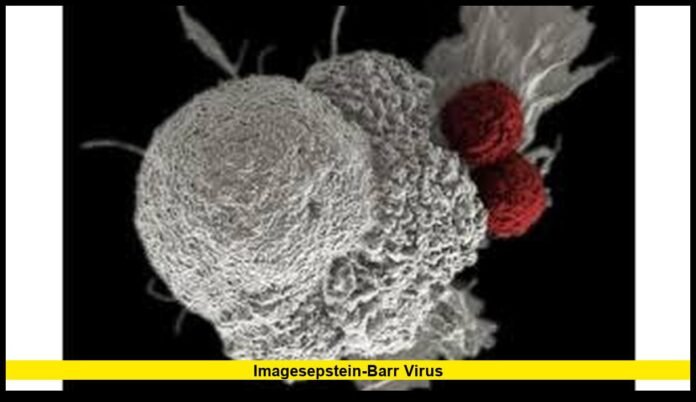
The Epstein Barr virus (EBV) has become the center of one of the most significant medical updates in years, reshaping how experts in the United States understand chronic illness, autoimmune disorders, and long-term viral impacts. With new research, clinical insights and public-health discussions emerging in 2025, EBV is no longer viewed only as the cause of mononucleosis—it is now recognized as a possible driving factor behind serious immune-related conditions that affect hundreds of thousands of Americans.
This growing body of evidence is drawing intense attention from U.S. researchers, clinicians, and patient communities, emphasizing the need to understand how EBV behaves in the body, why it activates decades after infection, and what can be done to detect, treat, or prevent EBV-linked complications.
Understanding the Widespread Nature of Epstein Barr Virus in the U.S.
EBV is one of the most common viral infections in the country, with the majority of people contracting it at some point—usually during childhood or adolescence. Once the body is infected, the virus remains for life in a dormant state, often without causing further symptoms. Because it spreads easily through saliva, casual contact in early life contributes to extremely high infection rates in the U.S. population.
While most individuals never develop serious complications, EBV’s ability to stay inside certain immune cells has made scientists question for years whether it plays a deeper, more harmful role in chronic disease. Now, emerging evidence is providing clearer answers—and some of them are changing medical perspectives.
New Evidence Connecting EBV to Lupus
Over the past year, a breakthrough in autoimmune research has linked Epstein Barr virus to Systemic Lupus Erythematosus, a chronic condition that affects hundreds of thousands of people in the United States. Researchers found that when EBV infects specific immune cells—particularly B cells—it can alter how those cells function. In individuals predisposed to autoimmune conditions, this interaction may encourage the immune system to mistakenly attack healthy tissues, producing inflammation across organs such as the skin, kidneys, joints, and lungs.
This finding is significant because lupus has long been considered a mysterious illness with unclear origins. The new evidence gives scientists a more precise mechanism to study and may lead to targeted therapies designed to address EBV-infected immune cells directly rather than relying solely on broad-spectrum immune suppression.
The impact is especially meaningful for women in the United States, as lupus disproportionately affects them—especially women of color, who experience higher rates and more severe complications. Understanding the viral trigger offers hope for earlier detection and more individualized treatments.
How EBV Affects the Immune System
EBV is known for its ability to hide within the immune system. After the initial infection, the virus settles into B cells—white blood cells vital for producing antibodies. In most people, the virus remains dormant, kept under control by the immune system. However, in some individuals, the virus may reactivate or modify cell behavior in ways that encourage inflammation or immune confusion.
Key immune-related changes include:
- Altered B-cell signaling
- Increased production of inflammatory proteins
- Activation of genes tied to chronic immune response
- Disruption of normal antibody function
- Long-term immune stress or overactivation
These effects are not always obvious, but they become important when someone either has a genetic vulnerability to autoimmune disease or experiences environmental stressors that weaken immune regulation.
Growing Clinical Attention in the United States
Healthcare providers in the U.S. are increasingly aware of EBV’s connection to a range of chronic conditions beyond lupus. This includes:
- Certain lymphomas
- Some neurological conditions with inflammatory features
- Chronic fatigue-related illnesses
- Post-transplant complications
- Potential links to long-term immune dysfunction
Clinics specializing in immunology and rheumatology have begun integrating EBV discussions into patient evaluations, especially when symptoms overlap multiple systems or show patterns commonly seen in chronic autoimmune illnesses.
Additionally, transplant centers across the country are paying close attention to EBV status in both donors and recipients. Individuals undergoing organ transplantation are at higher risk of complications if EBV reactivates during immune suppression. As a result, careful EBV monitoring is becoming more common.
Current Treatment Approaches and What May Come Next
There is no approved treatment specifically designed to eliminate Epstein Barr virus from the body. Instead, medical care focuses on:
- Controlling symptoms
- Regulating immune overreaction
- Managing inflammation
- Preventing organ damage
- Monitoring for complications
However, with new scientific insights emerging, the medical community is moving toward more targeted therapy ideas. These include:
- Treatments that deactivate EBV-infected B cells
- Therapies that block viral proteins believed to trigger autoimmune reactions
- Strategies to prevent EBV from reactivating in high-risk patients
- Better diagnostic tools to identify viral activity inside immune cells
EBV-focused treatments are still in development stages, but the expanding knowledge base is creating momentum that may lead to clinical trials in the near future.
Why Lupus Research Is Transforming EBV Understanding
The most transformative insight in recent years came from studies showing how EBV-infected B cells behave in individuals with lupus. Scientists discovered that these cells are far more common in lupus patients than in the general population, suggesting that the virus doesn’t just coexist with the disease—it may play an active role.
Important takeaways from these findings include:
- EBV-infected B cells appear to accelerate autoimmunity
- The virus may activate pathways that trigger inflammatory gene expression
- Some immune cells lose their ability to tell the difference between viral proteins and the body’s own proteins
- EBV may act as a spark in genetically predisposed individuals
These discoveries have inspired renewed focus on EBV in U.S. medical research, with multiple institutions now prioritizing EBV-related autoimmune studies.
How EBV Research Affects Public Health in America
Because EBV infects most people early in life, the virus has major public-health implications. The new research suggests that preventing EBV infection—or controlling reactivation—may one day significantly reduce the risk of autoimmune diseases.
Potential future strategies in the U.S. could include:
- Developing an EBV vaccine
- Screening high-risk groups for viral activity
- Creating immune-profiling tests for those with autoimmune tendencies
- Using genetic markers to predict EBV-related immune responses
- Offering early intervention for individuals showing abnormal EBV-linked immune activity
While these ideas are still in early exploration, the momentum in research makes them plausible long-term goals.
Practical Guidance for Americans Concerned About EBV
Although many people will carry EBV without complications, awareness of symptoms and risk factors is beneficial. Individuals should consider speaking with a healthcare provider if they experience:
- Recurrent severe fatigue
- Chronic swollen lymph nodes
- Joint pain or unexplained inflammation
- Rashes or sun-sensitivity
- Persistent fever
- A family history of autoimmune disorders
Those with lupus or other autoimmune diseases should discuss whether EBV could be influencing their symptoms or disease progression. Similarly, people who have undergone organ transplantation or receive long-term immunosuppressive therapy should regularly check in regarding EBV monitoring.
Final Outlook: What Americans Should Expect in the Coming Years
The Epstein Barr virus has been studied for decades, but recent discoveries have elevated it from a common childhood infection to a possible root cause of serious long-term disease. In the United States, this shift is already influencing research funding, clinical awareness, and conversations about preventive medicine.
Scientists are working toward greater clarity on why the virus affects people differently, how to prevent it from triggering immune complications, and what treatments may best protect those who are vulnerable. With ongoing developments, EBV may become one of the most important areas of immune-related research in this decade.
Share your thoughts or stay connected, as new updates on this evolving EBV story continue to unfold.