Health officials across the United States are once again urging people to pay close attention to mpox symptoms as new clusters of infections emerge in several states this October. Although the nationwide outbreak of 2022 is well behind us, mpox has not disappeared. The virus continues to circulate at low levels, with occasional spikes in transmission, making early recognition of symptoms a critical part of controlling its spread.
For many, the first signs of mpox can be confusing or easily mistaken for other illnesses. Understanding how the infection progresses, what to look for, and when to seek medical attention is essential to prevent further transmission and protect vulnerable communities.
What Is Mpox and Why Symptoms Matter
Mpox, formerly known as monkeypox, is a viral disease caused by the mpox virus, which is related to the virus that causes smallpox. Although generally less severe than smallpox, mpox can still lead to significant illness, pain, and complications—especially in individuals with weakened immune systems, pregnant people, and young children.
The virus spreads mainly through close, prolonged skin-to-skin contact, respiratory droplets during intimate or extended interactions, and contact with contaminated materials such as bedding, towels, or clothing.
Symptoms are the earliest warning sign that someone may be infected, often appearing before test results are available. Recognizing mpox symptoms early allows people to isolate quickly, receive supportive care, and reduce the risk of infecting others.
Early Mpox Symptoms: The First Warning Signs
After someone is exposed to the mpox virus, symptoms typically appear within 3 to 17 days. This incubation period means that a person might feel fine for over a week before noticing anything unusual.
Early symptoms can feel similar to a mild flu or another viral illness, but there are some key differences. The most common early mpox symptoms include:
- Fever – often the first noticeable sign, lasting 1–2 days before rash onset.
- Headache – can be intense and persistent.
- Chills and muscle aches – typical of the body fighting infection.
- Fatigue or malaise – a generalized feeling of weakness and exhaustion.
- Swollen lymph nodes – particularly in the neck, armpits, and groin. This is one of the most distinctive early signs that separates mpox from illnesses like chickenpox or measles.
In some individuals, especially during recent U.S. outbreaks, swollen lymph nodes may precede fever and rash, providing a critical early detection opportunity.
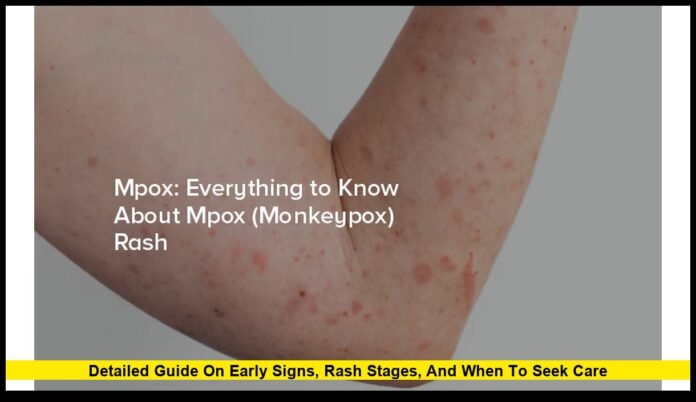
The Mpox Rash: Stages and Characteristics
The hallmark of mpox is its distinctive rash, which develops shortly after the initial flu-like symptoms. Typically, the rash appears 1 to 4 days after the onset of fever, but in some cases, lesions may be the first or only sign of infection.
The rash progresses through several well-defined stages:
- Macules – flat, discolored spots that mark the beginning of the rash.
- Papules – raised, firm bumps that develop from the macules.
- Vesicles – small fluid-filled blisters, often itchy or uncomfortable.
- Pustules – pus-filled lesions that can be painful, sometimes with a dimple in the center.
- Scabs – lesions crust over and eventually fall off, signaling the end of the contagious period.
Lesions typically evolve synchronously, meaning they all tend to be in the same stage of development across affected areas—unlike chickenpox, where lesions appear in different stages simultaneously.
Rash Distribution
- In many 2022–2025 U.S. cases, the rash began in localized areas, particularly the genital or perianal region, then sometimes spread to other parts of the body.
- Other common locations include the face, hands, feet, and chest.
- Some individuals develop only a few lesions, while others experience widespread rash over large areas of skin.
Rashes may last for 2 to 4 weeks, and individuals remain contagious until every scab has fallen off and new skin has formed.
Duration of Illness and Recovery
For most healthy individuals, mpox is a self-limited illness lasting between 2 and 4 weeks. Symptoms gradually improve without the need for hospitalization. Supportive care focuses on pain relief, hydration, and keeping lesions clean to prevent secondary infections.
However, contagiousness persists until all scabs are gone. Because this can take several weeks, public health officials recommend isolation at home for the entire duration of symptoms to prevent further spread.
Severe Mpox Symptoms and Complications
While many people experience mild to moderate illness, mpox can lead to more serious complications in some groups, including people with weakened immune systems, children under eight, and pregnant individuals.
Possible complications include:
- Painful proctitis (inflammation of the rectum), which can occur when lesions develop in the anal area.
- Secondary bacterial infections of lesions, especially if scratched or not kept clean.
- Severe dehydration in individuals with extensive lesions or difficulty swallowing.
- Eye complications, such as corneal infection, if lesions spread near the eyes.
- Pneumonia, sepsis, or encephalitis in rare, advanced cases.
Severe mpox requires medical evaluation. Antiviral treatments, such as tecovirimat (TPOXX), are available for patients at risk of complications or experiencing severe disease.
Mpox Symptoms vs. Other Common Illnesses
Because mpox symptoms can resemble other conditions, particularly chickenpox, shingles, or even certain sexually transmitted infections, accurate diagnosis is essential.
Here’s a quick comparison to help distinguish mpox from similar illnesses:
| Symptom | Mpox | Chickenpox | Shingles |
|---|---|---|---|
| Fever before rash | Common | Common | Rare |
| Lymph node swelling | Prominent | Rare | Rare |
| Rash progression | Uniform stage evolution | Mixed stages simultaneously | Localized to one nerve pathway |
| Rash location | May start in genital, face, hands | Typically trunk, face | Usually localized, unilateral |
| Duration | 2–4 weeks | 1–2 weeks | 2–4 weeks |
Swollen lymph nodes and synchronous lesion development remain two of the most important clinical clues for identifying mpox early.
Current U.S. Situation
As of October 2025, several states—including California, New York, Texas, and Illinois—have reported small but notable increases in mpox cases. The majority are linked to localized community transmission, with some associated with travel abroad.
The Centers for Disease Control and Prevention (CDC) continues to recommend vaccination for high-risk groups, early testing for anyone with suspicious rashes, and rapid treatment initiation for severe cases. Public health officials emphasize that awareness of mpox symptoms remains critical in preventing larger outbreaks.
When to Seek Medical Care
Anyone who develops symptoms consistent with mpox should contact a healthcare provider for evaluation. Testing involves swabbing lesions to confirm infection. Medical care is especially important if:
- You have lesions in sensitive areas, such as the eyes or genitals.
- You are immunocompromised or pregnant.
- You are experiencing severe pain or signs of secondary infection (redness, pus, swelling).
- You have difficulty breathing, swallowing, or controlling pain.
Prompt diagnosis and appropriate isolation are key steps in protecting both the patient and their community.
Prevention and Protection
While recognizing mpox symptoms is crucial, prevention remains the best defense. Health experts recommend the following steps:
- Vaccination – The JYNNEOS vaccine remains available for individuals at higher risk. Completing both doses provides strong protection.
- Avoid close contact with individuals who have unexplained rashes or mpox-like symptoms.
- Practice good hygiene, including frequent handwashing with soap and water.
- Use protective barriers, such as masks and gloves, during prolonged close interactions with someone who may be infected.
- Disinfect bedding, clothing, and surfaces that may have been contaminated by lesions.
Mpox Symptoms in Children and Special Populations
While most U.S. cases have occurred among adults, mpox can affect children and pregnant people as well.
- Children may develop more widespread rash and are at greater risk for complications like dehydration and bacterial infections.
- Pregnant individuals face risks of more severe disease and rare complications, including transmission to the fetus.
Special care and early medical intervention are critical for these groups.
Vaccination and Early Intervention
Vaccination plays a crucial role in reducing both symptom severity and transmission risk. Individuals who are vaccinated after exposure may still develop mpox, but symptoms are often milder and resolve more quickly.
Healthcare providers emphasize that recognizing early symptoms and seeking care promptly can prevent complications and limit spread to others.
Closing Thoughts
Understanding mpox symptoms is one of the most effective ways to detect cases early and prevent wider outbreaks. By knowing the early warning signs—particularly fever, lymph node swelling, and the distinctive rash—individuals can take swift action to protect themselves and others.
As new clusters emerge in the U.S., vigilance remains essential. Prompt medical evaluation, vaccination for those at risk, and continued public awareness will help keep mpox under control while ensuring those affected receive timely care.
Staying informed isn’t just about personal health—it’s about safeguarding communities across the country.